When you think of someone going into anaphylactic shock, what comes to mind? For me, it was always someone eating some sort of nut and then immediately swelling up not being able to breathe. Like it’s often portrayed in the movies, right? Well, now that I have experienced it first hand with my four-year-old, that couldn’t be farther from the truth. Yes, swelling can happen, but often there are other signs that most people wouldn’t necessarily look for when it comes to anaphylaxis.
These are the remnants I found left on the floorboard in my car from the next day after the first time having to use the epi- pen on my oldest child. He was having a reaction when I picked him up from school that day. The only signs he had were watery eyes and sneezing. These symptoms would be considered normal for this time of year. With the seasons changing right now, the pollen is in the air and seems to be affecting people more than usual. He ran up to me and immediately told me he didn’t feel good.
When we got to the car he was congested and also said he was having trouble breathing. At that moment, I knew he was having a reaction to something; I just didn’t know what was causing it. I gave him a dose of Benadryl and we headed to the urgent care right around the corner. By the time we got there, we had a new symptom. He now had hives on his face. While a nurse helped me hold him down, I injected him with epinephrine right there in the middle of the parking lot. We then rushed to the emergency room.
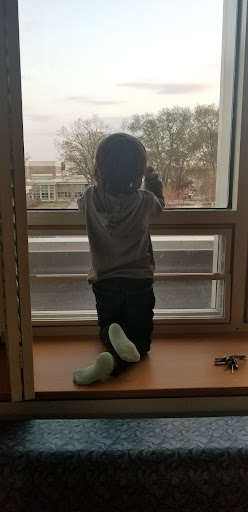
Once we got in, it was the busiest I had ever seen that lobby. While waiting in line to be checked in, he was acting pretty normal. He still had some congestion and he was super red (like he had spent the day on the beach with no sunscreen on). Once checked in they brought us back immediately, checked all his vitals, and got us into a room. They then hooked him up to a machine to monitor his blood pressure and oxygen levels.
While sitting in the room waiting to see the doctor, I was watching him closely because he was still so red and congested. I felt like his symptoms should have cleared up by now. A nurse came in and I expressed my concerns to her. We then lifted his shirt and his entire body was now covered in hives. She went to get some meds and a doctor, and while waiting for her to come back, he fell asleep.

In the middle of his nap, he started to have a secondary reaction which was far worse than the first. First, I noticed his oxygen levels dropping on the monitor. Then, he started stirring in his sleep. I knew something was wrong so I yelled for a nurse. At that time he woke up, told me he couldn’t breathe and needed a trash can. I brought the trash can over, he leaned his head over it, and went limp. I pulled him out and he had lost consciousness. He was as white as the hospital bed sheets and his fingers, toes, nose, and lips were turning blue. He was going in and out of consciousness for what seemed like forever.
While I’m still sitting here wondering why they didn’t give him another shot of epinephrine, he gained consciousness back on his own and they gave another dose of Benadryl and an oral steroid. They then admitted him to the children’s hospital for the night. They took an x-ray, did an EKG, and some blood work. All came back normal. By the time we got settled into our room at the children’s hospital, he was 99% back to his normal self.
They kept him overnight to monitor his oxygen levels, blood pressure, and pulse. The next morning they decided to give another dose of steroids, and by early Friday evening, we were discharged.
This event was, by far, the worst of all the reactions he’s had.
[The first time we had to epi him was this past Christmas Eve. He had gotten into a cheese pizza. After we gave the epi, his symptoms went away immediately. The doctor on call said not to even worry about taking him into the ER. ]
This reaction started around one o’clock in the afternoon and didn’t fully end until about five o’clock that evening. The signs and symptoms were not immediate. There was no swelling on his face or lips. His throat wasn’t closing. To someone who isn’t familiar with food allergies, they would’ve thought it was just the typical seasonal allergies. Every symptom was gradual, one after another. And while one epi injection should have done the trick, that’s not always the case. There can be secondary reactions.
While all of that was very terrifying at the moment, the most unnerving part of this reaction is not knowing what caused it. Did my child touch someone who had just been eating something he was allergic to? Did someone touch him without washing their hands? Did he touch a spot on the table where a piece of cheese was dropped before and not wiped down? Did he then put that same hand in his mouth? Was it something in the air? Did he develop a new allergy to something else? A million questions wondering what could’ve possibly happened, yet not one answer. I replay that day over and over trying to find an answer, but the reality of it is…there isn’t one. This is what parents with allergic children deal with on a day-to-day basis.
Living With anaphylaxis
Life with an allergy child, for me, is constant anxiety and overthinking. It is constant panic and overreacting over what should be normal everyday activities. I’m always wondering if a simple cough is just a cough or sneeze is just a sneeze; replaying the last couple of hours before it started. Sitting there waiting as the hour ticks by to see if he’s having any more symptoms. Is he going to have a reaction or not? Were we around anybody or anything that could’ve caused a reaction? Did someone have peanut butter on the playground? Did we wash his hands? Should I give him Benadryl? Should I wait? The mind of an allergy parent never stops. It is exhausting!
I try to carry most of this burden so that Nikolas can live as normal of a life as possible, but I can’t keep him in this protective bubble forever. I pray to God that he outgrows most of his allergies (if not all) so that he doesn’t have to live like this forever.
For now, I am going to be his strongest advocate. I am here to let it be known that food allergies are a serious matter. It isn’t a made up diagnosis. They can (and do) kill people, most being teenagers. Never in my life did I think I would be raising a child with allergies. I used to be that person that thought it was crazy that schools didn’t allow kids to bring peanut butter for lunch. I now, unfortunately, understand the importance of that rule. If it can protect and save a child’s life, it is a rule worth having. So next time your child is a part of a school or class with a “no nuts” rule, instead of complaining, replace the peanut butter with sunflower butter and take that time to thank the Lord that your child doesn’t have food allergies.
Being the parent to an allergy child is not an enjoyable task, but it is a part of our everyday life now. Labels need to be constantly checked. Hands and surfaces need to constantly be wiped and washed, especially out in public. The first aid bag can never be left at home and always needs to be easily accessible. Safe food options need to always be on hand because eating out is usually not an option. (Try eating breakfast out with a dairy allergic kid; it is next to impossible.) The list goes on, but I will continue to speak out for him and educate others on the seriousness of this subject. If you’ve made it to the end of this post, I have done my job on teaching you a little bit of what it is like in the world of allergies. So thanks for reading! Until next time…..
Resources:
https://www.aaaai.org/tools-for-the-public/anaphylaxis
https://www.mayoclinic.org/first-aid/first-aid-anaphylaxis/basics/art-20056608
Check out thehealthyplay.com for more articles.






